Why not consider a micro-invasive approach
for the treatment of urological disorders?

EchoLaser TPLATM SoracteLite is now part of ROCAMED SAM portfolio.
Please see Rocamed contact details in the CONTACTS page.
USA visitors must check the Legal Disclaimer at the end of this page

SoracteLite is the EchoLaser Thermal Ablation treatment for urological disorders.
The name of the treatment contains, in a single word, a reference to the urologic application (“Soracte” is the name of an Italian mountain – also named in the opening lines of a poem by Horace – where there was a monastery where the monk Nonnoso, canonised and considered the protector of people with kidney diseases, lived) and “Lite”, which refers, on one hand, to the lightweight and micro-invasive nature of the treatment, and, on the other, to the therapeutic source (Light, therefore Laser).
The name SoracteLite differentiates the procedure performed with ECHOLASER (micro-invasiveness and multi-fibre approach in a single system) from other thermal ablation techniques.
Suitability
SoracteLite is the EchoLaser Thermal Ablation for the treatment of benign and malignant urological disorders, namely Benign Prostatic Hyperplasia (BPH), low-risk localised Prostate Cancer (PCa), and Kidney Cancer.
Benign Prostatic Hyperplasia
SoracteLite is indicated for patients suffering from Benign Prostatic Hyperplasia – a disease in which the increase in volume of the prostate gland causes a compression effect on the bladder floor and the urethral channel – who choose not to undergo surgical treatment.
Prostate Cancer
The gold standard treatments for patients with low-risk localised prostate cancer are surgery or radiotherapy, but the side effects of the treatment and possible patient comorbidities might hamper patients to allow these kind of approaches. In such cases, as stated by the Guidelines on Prostate Cancer issued by medical associations in the America and Europe, Focal Therapy may be a therapeutic option to offer to those patients, preferably recommended within a clinical trial setting. Among the available Focal Therapies, SoracteLite Transperineal Laser Ablation (TPLATM) is a new Focal Laser Ablation (FLA) method that can destroy the lesion without causing the undesired side effects of radical therapies.
Kidney Cancer
As reported in the Guidelines issued by American and European urological associations, thermal ablative therapies have already been investigated as a possible alternative to surgery for the treatment of small and localized renal tumors (<4cm), with promising clinical results. This kind of approach is particularly suitable for patients at high surgical risk or with impaired renal function. In the field of minimally invasive therapies, SoracteLite applicators are considerably thinner than those used for radiofrequency ablation (RFA), microwave ablation (MWA) and cryoablation (CRA) devices currently on the market, ensuring an even less invasive approach, a key feature for patients at high risk of complications due to the presence of comorbidity (e.g. high risk of bleeding) or difficulty in technical access.
Performance
- Shrinkage of the enlarged prostate tissue volume with consequent relief from localised symptoms in patients with BPH, thanks to the Laser Induced CytoReduction (LICR) process
- Complete ablation of malignant tumors (Prostate or Kidney Cancer) with a sufficient safety margin
When you hear the word laser in urology, you instantly may think of surgical lasers, like the green laser. These lasers are an important step forward for endoscopic, transurethral surgery of the prostate. However, SoracteLite does not employ surgical lasers. Indeed, it differs from them in wavelength and power (EchoLaser employs 1064 nm wavelength and extremely low powers, 3-5 W) and in its mode of action. Lastly and most importantly, SoracteLite uses a truly micro-invasive approach (transperineal vs transurethral) with extremely thin needles (21G).
What is it?
SoracteLite for the treatment of BPH
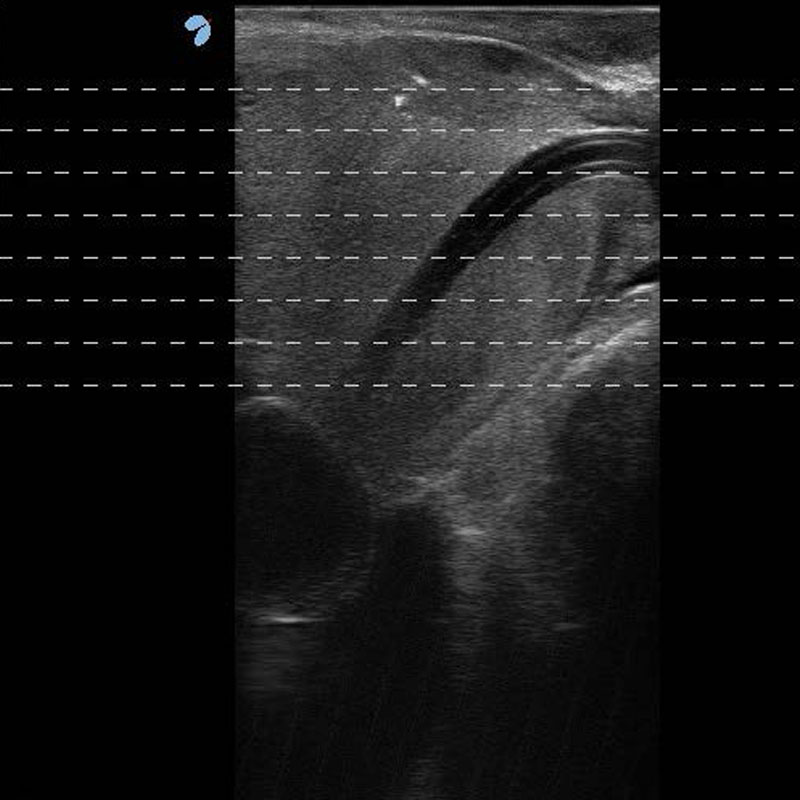
SoracteLite treatment consists in the percutaneous insertion of optical fibres (one or two fibres per lobe, depending on the basal volume of the prostate gland) via transperineal access (Transperineal Laser Ablation TPLATM), and the delivery of laser energy for several minutes, which heats the tissues until they are destroyed. This causes a progressive reduction in the volume of the prostate lobe (a volume reduction of at least 40% compared to the basal volume at one-year follow-up) and the subsequent disappearance of the symptoms. The planning of the treatment, the insertion of the needles and the monitoring are all carried out under ultrasound guidance.
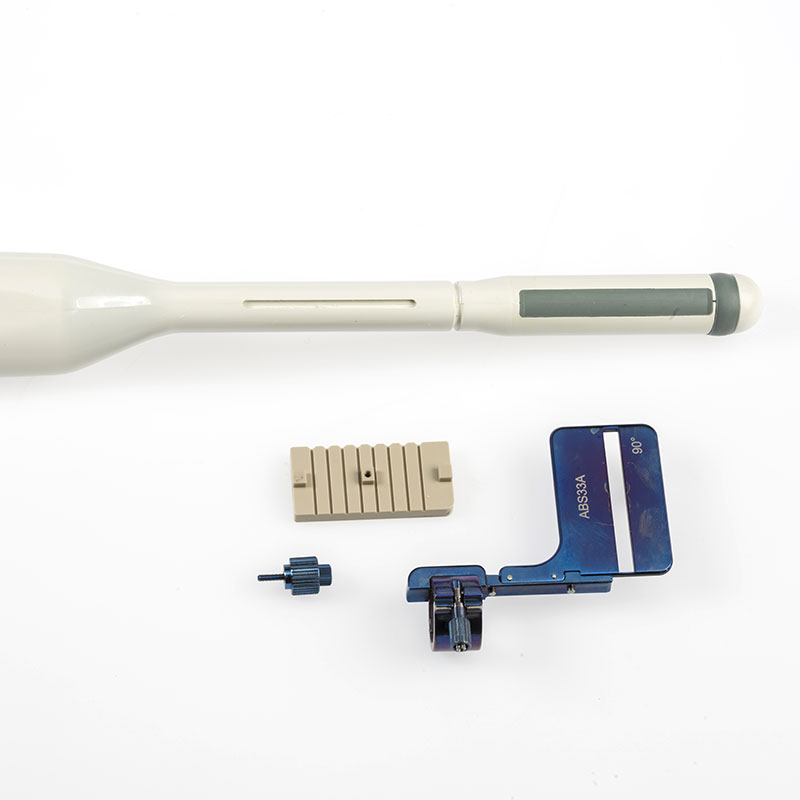
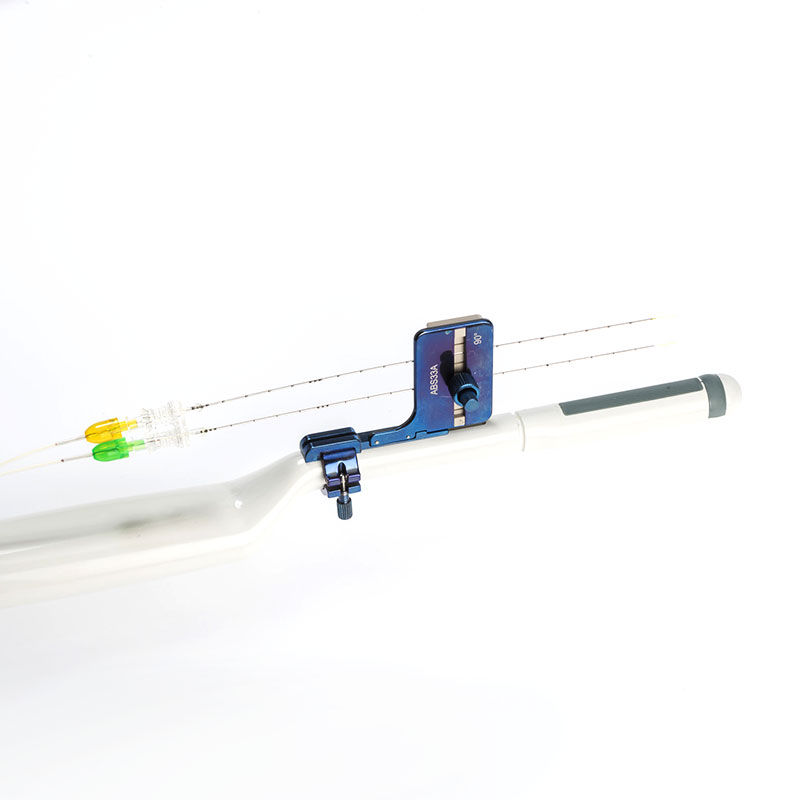
To facilitate insertion, the system has a dedicated transrectal ultrasound probe multi-applicator Guiding System with the relative Planning Software that displays the guidelines and the estimated ablation area on the ultrasound system screen.
With just one SoracteLite session it is possible to obtain a significant and persistent reduction of the prostate gland volume and an improvement of localised symptoms, without changing the prostate’s physiology.
1. TRT33 Esaote Probe with multi-fibre guiding system / 2. Biopsy Software
3./4. TRT33 Esaote Probe equipped with the multi-fibre guiding system
SoracteLite for the treatment of PCa
SoracteLite TPLATM (Transperineal Laser Ablation), a new Focal Laser Ablation method, consists in the percutaneous insertion of optical fibres via transperineal access under MRI-US Fusion Imaging guidance, and the delivery of laser energy for several minutes to heat the tissues until they are completely destroyed with a sufficient safety margin. The treatment is carried out with the use of needle guiding systems for the positioning of the applicators in the lesion, allowing to treat only the cancerous tissue, thus sparing the remaining healthy prostate.
With just one SoracteLite session it is possible to obtain the complete ablation of the lesion with sufficient safety margins, allowing the preservation of healthy tissue and the organ’s function.
SoracteLite for the treatment of Kidney Cancer
The optical fibres are inserted percutaneously to allow the heating of the tissues until they are completely destroyed with a sufficient safety margin. The positioning of the applicators, the monitoring of the treatment, and the verification of the effective coagulation area are carried out under ultrasound guidance. The insertion manoeuvre of the fibres is facilitated by dedicated multi-applicator guiding systems. As these are malignant tumors, the objective of the treatment is a complete ablation of the lesion and the subsequent absence of local post-treatment relapses.
With just one SoracteLite session it is possible to treat kidney tumors of a very wide size and diameter range, thanks to the versatility of the multi-fibre approach. The localised thermal effect of SoracteLite makes it a valuable alternative for patients at high risk of bleeding.
Advantages
transperineal approach (TPLATM)
gradual and constant relief from symptoms
thermal damage “in situ”
use of fine and atraumatic needles with transperineale approach
absence of general anaesthesia
short duration of treatment (few minutes)
fast recovery times
no or irrelevant post-treatment pain
absence of erectile dysfunction or complications related to the reproductive organs
For more details about the SoracteLite procedure, please visit the dedicated website: www.soractelite.info
Clinical Case no.1
Patient suffering from BPH, with a basal volume of 64 ml. Treated with two fibres per lobe.

US image before treatment
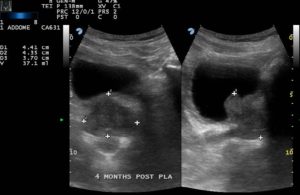
Four-month follow-up US image
The four-month follow up revealed the following:
- volumetric reduction from 64 ml to 37 ml
- post-urination residue reduction from 200 ml to 43 ml
- IPSS score reduction from 29 to 10
- Quality of Life (QoL) from 5 to 1
- Maximum flow speed up from 4 ml/s to 14 ml/s
- No complications
Images courtesy of Dr. Patelli (Pesenti Fenaroli Hospital, Alzano Lombardo)
Benign Prostatic Hyperplasia
- Transperineal laser ablation (TPLA) of the prostate for benign prostatic obstruction: the first 100 patients cohort of a prospective, single-center study. Lo Re M, Polverino P, Rivetti A, Pecoraro A, Saladino M, Pezzoli M, Siena G, De Nunzio C, Marzi VL, Gacci M, Serni S, Campi R, Sessa. World J Urol. 2024 Jul 10;42(1):402. doi: 10.1007/s00345-024-05077-z. PMID: 38985193
- Transperineal Laser Ablation of the Prostate for Symptomatic Benign Prostatic Hyperplasia: Long-Term Follow-Up in 40 Patients. Patelli G, Altieri VM, Ierardi AM, Carnevale A, Chizzoli F, Baronchelli G, Trimarchi R, Carrafiello G. Journal of Vascular and Interventional Radiology, 2024,ISSN 1051-0443, https://doi.org/10.1016/j.jvir.2024.04.023
- Office-Based Transperineal Laser Ablation for Benign Prostatic Hyperplasia Under Local Anesthesia: 2-Year Results from a Dose Range Confirmatory Trial. Bianco FJ, Luna E, Lopez-Prieto A, González P, Gheiler EL, Kaufman AM, Avila L, Maiolino G. JU Open Plus 2(2):e00007, February 2024. | DOI: 10.1097/JU9.0000000000000105
- Minimally invasive techniques in quest of Holy Grail of surgical management of enlarged prostates: a narrative review. Porto JG, Titus R, Camargo F, Bhatia A, Ahie N, Blachman-Braun R, Malpani A, Lopategui DM, Herrmann TRW, Marcovich R, Shah HN. World J Urol. 2024 Jan 13;42(1):35. doi: 10.1007/s00345-023-04747-8. PMID: 38217727.
- Could transperineal interstitial laser ablation of the prostate be the right option for highly comorbid patients with lower urinary tract symptoms due to benign prostatic obstruction? A preliminary single-center experience focusing on functional and safety outcomes. Polverino P, Lo Re M, Saladino S, Pecoraro A, Moscardi L, Rivetti A, Resta GR, Pezzoli M, Romano A, Somani BK, Siena G, Cocci A, Gacci M, Minervino A, Serni S, Campi R, Sessa F
- Minimally invasive surgical therapies (MISTs) for lower urinary tract symptoms (LUTS): promise or panacea? Busetto GM, Checchia A, Recchia M, Tocci E, Falagario U , Annunziata G , Annese P , d’Altilia N , Mancini V, Ferro M , Crocetto F , Tataru OS , Di Gianfrancesco L, Porreca A, Del Giudice F , De Berardinis E, Bettocchi C, Luigi Cormio, Carrieri G. Asian Journal of Andrology (2023) 25, 1–9; doi: 10.4103/aja202357
- Trans – Perineal laser ablation of the prostate in high surgical risk patients affected by severe lower urinary tract symptoms related to benign prostatic obstruction. Destefanis P, Sibona M, Vitiello F, Vercelli E, Micai L, Montefusco G, Mangione C, Bracco F, Colucci F, De Nunzio C, Gontero P. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00736-5
- Transperineal laser ablation as treatment for benign prostatic obstruction: Safety, feasibility and functional outcomes—A pilot study. van Kollenburg R, van Riel L, Bloemen P, de Reijke T, Beerlage H, de Bruin D et al. BJUI Compass. 2023. https://doi.org/10.1002/bco2.278.
- Transurethral resection of the prostate (TURP) versus transperineal laser ablation (TPLA) due to benign prostatic hyperplasia (BPH): prospective and comparative study. Canat HL, Gurbuz C, Bozkurt M. Int Urol Nephrol. 2023 Jul 27. doi: 10.1007/s11255-023-03717-8.
- Transperineal laser ablation of the prostate as a treatment for benign prostatic hyperplasia and prostate cancer: The results of a Delphi consensus project. Cocci A et al. Asian Journal of Urology, 2023, ISSN 2214-3882, https://doi.org/10.1016/j.ajur.2023.07.001.
- Three years outcomes of transperineal laser ablation of the prostate. Minafra P, DE Rienzo G, Gerbasi S, Cindolo L, Battaglia M, Ditonno P. Minerva Urol Nephrol. 2023 Jun 14. doi: 10.23736/S2724- 6051.23.05270-9. Epub ahead of print. PMID: 37314812.
- Ablative minimally invasive surgical therapies for benign prostatic hyperplasia: A review of Aquablation, Rezum, and transperineal laser prostate ablation. Nguyen DD, Li T, Ferreira R, Baker Berjaoui M, Nguyen AV, Chughtai B, Zorn KC, Bhojani N, Elterman D. Prostate Cancer Prostatic Dis. 2023 Apr 20. doi: 10.1038/s41391- 023-00669-z. PMID: 37081044.
- Ejaculatory Function following Transperineal Laser Ablation versus TURP for Benign Prostatic Obstruction: A Randomized Trial. Bertolo R, Iacovelli V, Cipriani C, Carilli M, Vittori M, Antonucci M, Maiorino F, Signoretti M, Petta F, Travaglia S, Panei M, Bove P. BJU Int. 2023 Mar 14. doi: 10.1111/bju.16008. PMID: 36917033.
- Transperineal Laser Ablation for Benign Prostatic Enlargement: A Systematic Review and Pooled Analysis of Pilot Studies. Tafuri A, Panunzio A, De Carlo F, Luperto E, Di Cosmo F, Cavaliere A, Rizzo M, Tian Z, Shakir A, De Mitri R, Porcaro AB, Cerruto MA, Antonelli A, Cormio L, Carrieri G, Karakiewicz PI, Abreu AL, Pagliarulo V. J Clin Med. 2023 Feb 26;12(5):1860. doi: 10.3390/ jcm12051860. PMID: 36902647; PMCID: PMC10003190.
- Ultrasound-guided SoracteLite™ transperineal laser ablation (TPLA) of the prostate for the treatment of symptomatic benign prostatic hyperplasia (BPH): a prospective single-center experience. Laganà A, Di Lascio G, Di Blasi A. et al. World J Urol (2023). https://doi.org/10.1007/ s00345-023-04322-1.
- Standard approach and future perspective for the management of benign prostatic hyperplasia from a health- economics point of view: the role of transperineal laser ablation. Lorenzoni V, Palla I, Manenti G, Ditonno P, de Reijke TM and Turchetti G. Front. Urol. 3:1100386. doi: 10.3389/fruro.2023.1100386.
- Transperineal Laser Ablation of the Prostate (TPLA) for Lower Urinary Tract Symptoms Due to Benign Prostatic Obstruction. Sessa F, Polverino P, Siena G, Bisegna C, Lo Re M, Spatafora P, Pecoraro A, Rivetti A, Moscardi L, Saladino M, et al. J. Clin. Med. 2023, 12, 793. https://doi.org/ 10.3390/ jcm12030793.
- Efficacy and safety of ultrasonography guided transperineal percutaneous laser ablation for treating benign prostatic hyperplasia: a randomized controlled trial. Chen L, Zhang W, Meng Z, Guo Q, Cao N, Xu Y, Fu Q, Hu B. https://doi.org/10.21203/rs.3.rs-2433606/v
- Ultrasound-guided perineal laser ablation versus prostatic arterial embolization for benign prostatic hyperplasia: two similar short-term efficacies. Cai H, Zhu C, Fang J. Acta Radiol. 2022 Nov 27:2841851221140214.
- Transperineal laser ablation of the prostate with EchoLaser™ system: perioperative and short-term functional and sexual outcomes. Sessa F, Polverino P, Bisegna C, Siena G, Lo Re M, Spatafora P, Pecoraro A, Rivetti A, Conte FL, Cocci A, Villari D, Minervini A, Gacci M, Li Marzi V, Serni S and Campi R. Front. Urol. 2:969208. doi: 10.3389/fruro.2022.969208.
- Transperineal laser ablation of the prostate (TPLA) for selected patients with lower urinary tract symptoms due to benign prostatic obstruction: a step-by-step guide. Sessa F, Bisegna C, Polverino P , Gacci M, Siena G , Cocci A , Li Marzi V, Minervini A, Serni S , Campi R. Urology Video Journal, Volume 15, 2022, 100167.
- Ultrasound-guided transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a new minimally invasive interventional therapy. Cai HJ, Fang JH, Kong FL, Xu CK, Chen CH, Wang W, Huang B. Acta Radiol. 2022 Apr;63(4):553-558.
- Feasibility, safety, and efficacy of ultrasound-guided transperineal laser ablation for the treatment of benign prostatic hyperplasia: a single institutional experience. Frego N, Saita A, Casale P, Diana P, Contieri R, Avolio PP, Lazzeri M, Hurle R, Buffi NM, Guazzoni GF, Lughezzani G. World J Urol. 2021 Oct;39(10):3867-3873.
- 3-T MRI and clinical validation of ultrasound-guided transperineal laser ablation of benign prostatic hyperplasia. Manenti G, Perretta T, Calcagni A, Ferrari D, Ryan CP, Fraioli F, Meucci R, Malizia A, Iacovelli V, Agrò EF, Floris R. Eur Radiol Exp. 2021 Sep 17;5(1):41.
- Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. De Rienzo G, Lorusso A, Minafra P, Zingarelli M, Papapicco G, Lucarelli G, Battaglia M, Ditonno P. Eur Urol. 2021 Jul;80(1):95-103.
- Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Results at 6 and 12 months from a retrospective multi-centric study. Pacella CM, Patelli G, Iapicca G, Manenti G, Perretta T, Ryan CP, Esposito R, Mauri G. Prostate Cancer Prostatic Dis. 2020 Jun;23(2):356-363.
- Transperineal Laser Ablation for Percutaneous Treatment of Benign Prostatic Hyperplasia: A Feasibility Study. Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Cardiovasc Intervent Radiol. 2017 Sep;40(9):1440-1446.
Prostate Cancer
- Transperineal Laser Ablation for Focal Therapy of Localized Prostate Cancer: 12-Month Follow-up Outcomes from a Single Prospective Cohort Study. Iacovelli V, Carilli M, Bertolo R, Forte V, Vittori M, Filippi B, Di Giovanni G, Cipriani C, Petta F, Maiorino F, et al. 2024; 16(15):2620. https://doi.org/10.3390/cancers16152620
- Transperineal Laser Ablation (TPLA) Treatment of Focal Low–Intermediate Risk Prostate Cancer. Manenti G, Perretta T, Nezzo M, Fraioli FR, Carreri B, Gigliotti PE, Micillo A, Malizia A, Di Giovanni D, Ryan CP, et al. Cancers. 2024; 16(7):1404. https://doi.org/10.3390/cancers16071404
- Transperineal laser ablation (TPLA) with ultrasound/MRI fusion guidance in the treatment of localized radiotherapy-resistant prostate cancer. Manenti G, Nezzo M, Ryan CP, Fraioli FR, Carreri B, Gigliotti PE, et al. BJR Open (2023) 10.1259/bjro.20230042.
- Transperineal laser ablation of the prostate as a treatment for benign prostatic hyperplasia and prostate cancer: The results of a Delphi consensus project. Cocci A et al. Asian Journal of Urology, 2023, ISSN 2214-3882, https://doi. org/10.1016/j.ajur.2023.07.001.
- Reliable Visualization of the Treatment Effect of Transperineal Focal Laser Ablation in Prostate Cancer Patients by Magnetic Resonance Imaging and Contrast- enhanced Ultrasound Imaging.Van Riel LAMJG, Van Kollenburg RAA, Freund JE, Almasian M, Jager A, Engelbrecht MRW, Smit RS, Bekers E, Nieuwenhuijzen JA, Van Leeuwen PJ, Van der Poel H, De Reijke TM, Beerlage HP, Oddens JR, De Bruin DM. European Urology Open Science, Volume 54, August 2023, Pages 72-79.
- A single-operator experience using EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer: One more arrow in the quiver for the conservative management of the disease. Meneghetti I, Giardino D, Morganti R, Marino V, Menchini Fabris F, Bartoletti R, Pinzi N. Archivio Italiano Di Urologia E Andrologia, 94(4), 406–412. https://doi.org/10.4081/aiua.2022.4.406.
- Safety and Feasibility of Soractelite Transperineal Focal Laser Ablation for Prostate Cancer and Short-term Quality of Life Analysis from a Multicenter Pilot Study. Van Riel L, van Kollenburg R , Andre´ N. Vis AN , van Leeuwen PJ , de Reijke TM , de Bruin DM , Oddens JR. Prostate Cancer| Volume 39, P48-54, May 01, 2022
Kidney Cancer
- Image-guided laser ablation in the treatment of recurrence of renal tumours: technique and preliminary results. Ferrari F, Mauri G, Nicosia L, Varano GM, Bonomo G, Orsi F. Eur Radiol Exp. 2020 Jan 3;4(1):1.
- Ultrasound-guided percutaneous laser ablation is safe and effective in the treatment of small renal tumors in patients at increased bleeding risk. Sartori S, Mauri G, Tombesi P, Di Vece F, Bianchi L, Pacella CM.
- Image-Guided Ablations in Patients with Recurrent Renal Cell Carcinoma. Aurilio G, Mauri G, Rossi D, Della Vigna P, Bonomo G, Varano GM, Maiettini D, Rocca MC, Verri E, Cullurà D, Nolè F and Orsi F. Journal of Clinical Medicine. 2023; 12(15):4902. https://doi. org/10.3390/jcm12154902.
- CT-guided percutaneous laser ablation of adrenal metastases from kidney cancer. Oltmanns G. P167 – ECIO 2023 Book of Abstracts. Cardiovasc Intervent Radiol 46 (Suppl 2), 23–271 (2023). ttps://doi.org/10.1007/ s00270-023-03414-0.
- Image-guided laser ablation in the treatment of recurrence of renal tumours: technique and preliminary results. Ferrari F, Mauri G, Nicosia L, Varano GM, Bonomo G, Orsi F. Eur Radiol Exp. 2020 Jan 3;4(1):1. doi: 10.1186/s41747-019- 0127-0.
SoracteLite procedure for the treatment of Benign Prostatic Hyperplasia
SoracteLite procedure for the focal laser ablation of Prostate Cancer
Transperineal Laser Ablation for Low- and Intermediate Risk Prostate Cancer: a Single Cohort Analysis
- No. of Patient: 20
- Reference centre of the study: Ospedale San Carlo di Nancy, Rome
- State of the Study: Follow-Up
- Registration link: https://clinicaltrials.gov/ct2/show/NCT05584787
Transperineal Laser Ablation for Treatment of LUTS Due to Benign Prostatic Obstruction
- No. of Patient: 20
- Reference centre of the study and Sponsor: Academisch Medisch Centrum – Universiteit van Amsterdam (AMC-UvA)
- State of the Study: Completed
- Registered on ClinicalTrial.gov: https://clinicaltrials.gov/ct2/show/NCT03653117
Registry of Transperineal Laser Ablation for Treatment of Lower Urinary Tract Symptoms With Use of the Echolaser® Device: A Multicentre, International Registry to Evaluate the Treatment of Lower Urinary Tract Symptoms in Terms of Long-term Efficacy, Functional Outcomes and Safety
- No. of Patient: 500
- Sponsor: Academisch Medisch Centrum – Universiteit van Amsterdam (AMC-UvA)
- State of the Study: patients recruitment
- Registered on ClinicalTrial.gov: https://clinicaltrials.gov/ct2/show/NCT03776006
Efficacy of Ultrasound Guided Percutaneous Transperineal Laser Ablation in Benign Prostatic Hypertrophy Patients: Non-Pharmacological Interventional Study
- No. of Patient: 40
- Reference centre of the study: Ospedale Tor Vergata, Roma
- State of the Study: Completed
- Registered on ClinicalTrial.gov: https://clinicaltrials.gov/ct2/show/NCT04044573
Tolerability of percutaneous ablation Neodymium Laser in patients suffering from Benign Prostatic Hyperplasia (BPH): Prospective Observational Pilot Study
- No. of Patient: 10
- Reference centre of the study: Ospedale Pesenti Fenaroli, Alzano Lombardo (BG)
- Sponsor: Dr. Gianluigi Patelli
- State of the Study: Completed
Transperineal Laser Ablation for Benign Prostatic Hyperplasia with Bladder Outlet Obstruction
- No. of Patient: 20
- Reference centre of the study: Urology Specialist Group, Miami Florida
- State of the Study: Completed
- Registered on ClinicalTrial.gov: https://www.clinicaltrials.gov/ct2/show/NCT04760483
Transperineal Laser Ablation for Treatment of LUTS Due to Benign Prostatic Obstruction
- No. of Patient: 140
- Reference centre of the study: Shanghai Sixth People’s Hospital, China
- State of the Study: patients recruitment
- Link of registration of the Clinical Trial: http://www.chictr.org.cn/showproj.aspx?proj=34314
Trans-perineal laser ablation of prostate adenoma for the micro-invasive treatment of obstructive symptoms from benign prostatic hypertrophy: Randomized clinical study of comparison with transurethral prostate resection (TURP)
- No. of Patient: 50
- Reference centre of the study: Ospedale San Carlo di Nancy, Roma
- State of the Study: patients recruitment
- Link of registration of the Clinical Trial: https://www.clinicaltrials.gov/ct2/show/NCT04781049
Short-term efficacy of transperineal laser ablation with image fusion in prostate cancer patients: Multidisciplinary interventional pilot study
- No. of Patient: 30
- Reference centre of the study: Ospedale Tor Vergata, Roma
- State of the Study: Completed
- Link of registration of the Clinical Trial: https://www.clinicaltrials.gov/ct2/show/NCT04045756
Transperineal laser ablation for focal treatment of prostate cancer: the safety and ablative efficacy of transperineal laser ablation for focal prostate cancer treatment compared with radical prostatectomy histological analysis
- No. of Patient: 12
- Reference centre of the study and Sponsor: Academisch Medisch Centrum – Universiteit van Amsterdam (AMC-UvA)
- State of the Study: Completed
- Registered on ClinicalTrial.gov: https://www.clinicaltrials.gov/ct2/show/NCT04170478
Transperineal Laser Ablation Treatment for Prostate Cancer Registry: a Retrospective and Multicenter Evaluation
- No. of Patient: 200
- Reference centre of the study and Sponsor: Academisch Medisch Centrum – Universiteit van Amsterdam (AMC-UvA)
- State of the Study: patients recruitment
- Registered on ClinicalTrial.gov: https://www.clinicaltrials.gov/ct2/show/NCT05163197